At my last botox appointment, my Neuro asked me about my chronic migraine status. Sometimes keeping track of Chronic Migraine can be so completely depressing, so I admit I’ve slacked off on my tracker phone apps. But I thought a bit about my recent experiences before answering the question… I realized that while I have migraine symptoms every single day (🙄 of course… photophobia, lethargy, pain, phonophobia, brain fog, and so much more), I really only have about 2 migraine episodes a week that last approximately ~24 hours with treatment. This is an exceptional improvement, for sure. And I truly am grateful 🙌🏼
This solid progress is is a result of my Chronic Migraine regimen right now: •Botox every 12 weeks, •Nurtec (as a preventive) every other morning, •Nadolol 10mg and Tizanidine 4mg every night. For abortive treatment, I still have a plethora to cycle: Reyvow, Maxalt, Ubrelvy, Butalbitol, Sumatriptan injection, Phenergen, Indomethacin.
However, some very SAD news in my migraine world: Reyvow is being pulled because it isn’t making enough money for the company. I’m so unhappy: I really, really like Reyvow for those particularly bad or nighttime migraines… so I’m trying to fill my script as much as possible before the medication sunsets forever.
Discontinuation of Reyvow® (lasmiditan) for Acute Migraine Treatment: What To Do Next – Association of Migraine Disorders https://share.google/RrDGctNMDlPP7hmX0
While I was thrilled to acknowledge this solid Migraine win, my buddies Rheumatoid Arthritis and Sacroiliac Joint Dysfunction still are a huge part of my Chronic Illness daily life. And they never let me forget it!
Love you all… Warriors: keep up the fight!💪🏼💜


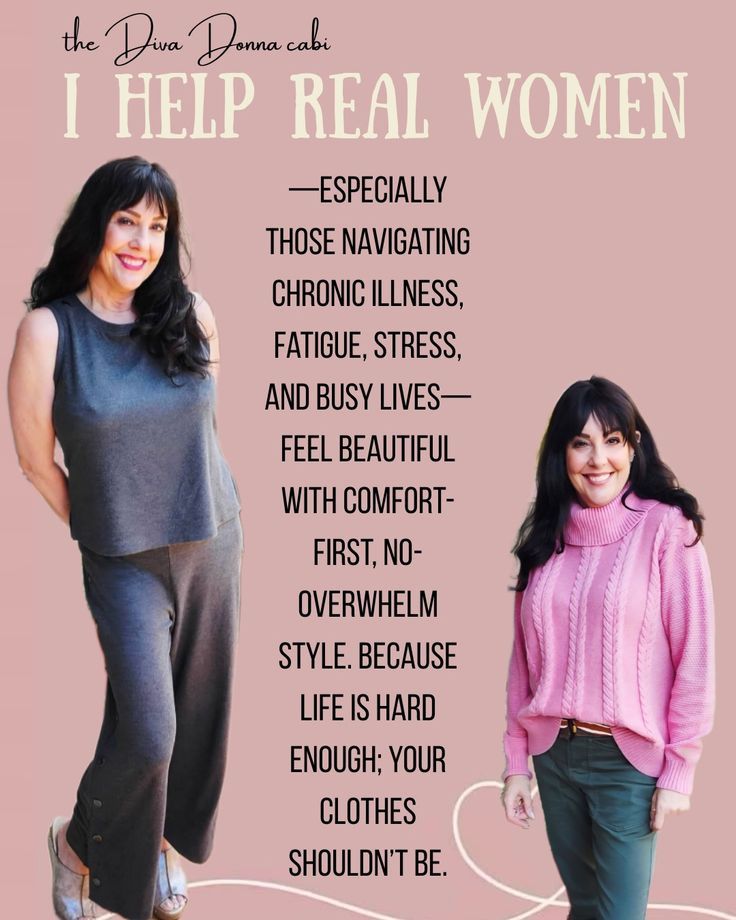
Still overwhelmed trying to work my biz… but it’s amazing for feeding my soul to serve women, flexibility and honoring friendships.
https://cabi.cabionline.com/TheDivaDonna




Of course as I type this, I’m quite sick with a head cold. It’s not the flu, it’s not very serious, but having “just a cold” while battling Chronic Illness and a compromised immune system is the ultimate injustice! I’ve been incapacitated the last 5 days and hope tomorrow is a better day!😊
















